Nearly two years after the WHO declared COVID-19 a global pandemic, researchers are still learning more about how the virus has affected clinical and pharmaceutical research.
By Emily Newton
COVID-19’s impact could have significant long-term consequences for a variety of research industries.

This is what we know now about the virus’s impact on labs and how the pandemic may be reshaping the future of research.
The Immediate Impact of COVID-19 on Labs
Coronavirus Disease 2019 (COVID-19) was formally characterized as a pandemic by the WHO on March 11, 2020. Almost immediately, many non-medical labs were forced to shutter, while medical labs found themselves facing a wave of “unprecedented demand” for healthcare resources, including medical testing.
At the same time, however, non-COVID testing dropped precipitously. In the second quarter of 2020, smaller labs reported a 40 to 90% reduction in testing volumes, and some in vitro fertilization labs shuttered entirely.
Larger labs, in general, tended to fare better — but did not escape COVID’s impact. Big box labs reported a 40% drop in testing volumes.
The drop in demand was not evenly distributed across different types of testing not related to COVID-19. Pathology and toxicology testing volume, for example, dropped by 50%, while non-invasive prenatal screening for fetal chromosome conditions dropped by only 20%.
The only tests that saw volume increase during the early days of the pandemic were related to COVID-19 — like testing for interleukin-6, a cytokine that appears to serve as a predictor of severe disease in COVID patients. Demand for these tests sometimes surged well above pre-pandemic levels.
Many medical laboratories also secured additional testing equipment to meet these new demands. In some cases, laboratories began using molecular testing tools for the first time.
According to data from the Association of Public Health Laboratories, a small-but-significant portion of public health labs (PHLs) struggled to keep up with demand for COVID-19 testing. It was only in mid-2021 that 100% of PHLs were able to consistently meet this testing demand.
A minority of PHLs also struggled (and continue to struggle) with reagent shortages and supply chain disruptions.
How COVID-19 May Change Lab Design and Management
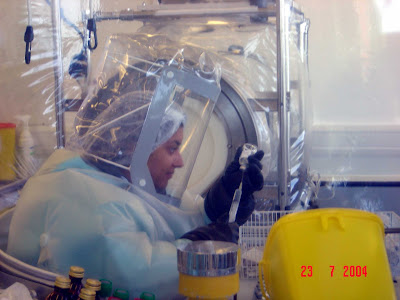
After the WHO’s declaration of the COVID-19 pandemic, and in the months that followed, laboratories of all kinds adopted new policies — like mandatory PPE and social distancing — intended to combat the spread of COVID in their facilities without fully shutting down their facilities.
New lab habits and protocols emerged as lab managers looked to limit the spread of COVID while grappling with labor shortages and supply shocks that made effective safety protocols harder to implement.
For example, many hospitals “set up methods for reprocessing and disinfecting gowns and N95 respirators for reuse using ultraviolet lighting or a hydrogen peroxide vapor treatment,” according to lab safety expert Dan Scungio writing for Lab Manager Magazine.
Many laboratories switched from using disposal lab gowns and coverings to reusable ones. These same labs also quickly developed new protocols for COVID-19 testing and had discussions about room ventilation, safety equipment, and specimen transport.

Scungio concluded that a year after the pandemic began, “fear among lab workers appears to be diminished. Proper procedures are in place, and adequate protection measures have been implemented.”
In addition to mitigating the spread of COVID-19, changes to lab practices could also help to make labs safer and more efficient in general.
For example, safety policies, reusable PPE, and improved ventilation can all help to prevent the spread of other infectious diseases, as well as limit worker exposure to toxic fumes and dangerous chemicals that can be a major safety risk in lab environments.
Ongoing PPE shortages and supply chain disruptions will continue to make certain safety practices challenging to implement — and experts believe that it may be years before supply chain experts are able to expand production capacity and leverage technology like AI to resolve current supply chain issues.
However, in the long term, the pandemic could help to make medical labs much safer work environments.
As the Pandemic Continues, What’s Next for Laboratories?
Right now, COVID-19 case rates are declining, and Omicron — a variant that is much more transmissible than previous variants but appears to cause less severe disease — remains the dominant COVID variant.
Some disease experts and pharmaceutical industry leaders believe that the pandemic could be close to over — though others remain wary of future variants that could be more transmissible, more virulent, and better at escaping vaccine immunity.
In the short term, demand for COVID-19 testing will remain high while other types of testing could remain below expected levels. Essential laboratory resources, like reagents and PPE, may remain more expensive or more challenging to source than they were before the pandemic.
Over the next few years, the long-term impact of the pandemic will become more clear. It’s likely that COVID-19 could change how lab managers approach safety and lab design.
Lab managers and staff may also use their experience with COVID-19 to prepare for future crises. Future PPE shortages could have less of an impact on the industry now that many laboratories have adopted reusable personal protective equipment.
Pharmaceutical Microbiology Resources (http://www.pharmamicroresources.com/)


No comments:
Post a Comment
Pharmaceutical Microbiology Resources