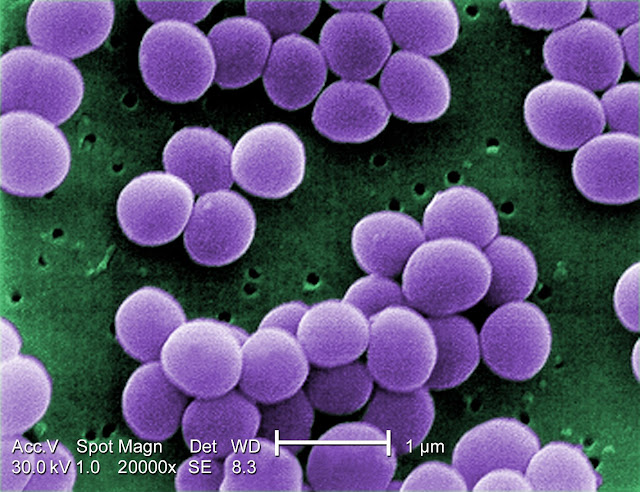
A new analysis reveals how Staphylococcus aureus gains mutations that allow it to colonize eczema patches. The findings provide direct evidence of adaptive evolution in the skin microbiome.

Scientists from Massachusetts Institute of Technology have discovered that Staphylococcus aureus can rapidly evolve within a single person's microbiome. With people with eczema, S. aureus tends to evolve to a variant with a mutation in a specific gene that helps it grow faster on the skin.
While human skin is home to millions of microbes, S. aureus is found on many people as an opportunistic pathogen that can invade patches of skin affected by eczema (atopic dermatitis).
It is estimated that between 30 and 60 percent of people carry S. aureus in their nostrils. Here it is usually harmless. However, for people with eczema, S. aureus often spreads to eczema patches and infects the skin by finding a niche where the bacterium can grow and replicate.
Upon infection, S. aureus evolves to a variant with a mutation in a specific gene that helps it grow faster on the skin. Such bacteria contribute to the pathology because they secrete toxins and recruit immune cells, and this immune reaction further damages the skin barrier.
Data was gathered from samples taken of patients aged 5 to 15 who were being treated for moderate to severe eczema, across nine months. Samples were taken from the backs of the knees and inside of the elbows (the most common sites affected by eczema), the forearms, which are usually not affected, and the nostrils.
The researchers sequenced the cells' genomes. This yielded nearly 1,500 unique colonies, enabling observations about the bacterial cells' evolution to be made. This showed that most patients maintained a single lineage of S. aureus (hence it was very uncommon for a new strain to come in from the environment or another person and replace the existing S. aureus strain). Yet within each lineage, mutation and evolution occurred during the nine months of the study.
Many of these mutations arose in a gene called capD, which encodes an enzyme necessary for synthesizing the capsular polysaccharide -- a coating that protects S. aureus from recognition by immune cells. In two out of six deeply sampled patients, cells with capD mutations took over the entire S. aureus skin microbiome population.
Mutations to capD allowed S. aureus to grow faster than S. aureus strains with a normal capD gene. This is because synthesizing the capsular polysaccharide requires a lot of energy, so when cells do not have to make it, they have more fuel to power their own growth. It is also hypothesized that loss of the capsule may allow the bacteria to stick to the skin better because proteins that allow them to adhere to the skin are more exposed.
The researchers later analyzed nearly 300 publicly available genomes of bacteria isolated from people with and without eczema and found that people with eczema were much more likely to have S. aureus variants that could not produce the capsular polysaccharide than people without eczema.
The findings could help researchers develop potential treatments that would soothe the symptoms of eczema by targeting variants of S. aureus that have this type of mutation.

Felix M. Key, Veda D. Khadka, Carolina Romo-González, et al. On-person adaptive evolution of Staphylococcus aureus during treatment for atopic dermatitis. Cell Host & Microbe, 2023; 31 (4): 593 DOI: 10.1016/j.chom.2023.03.009
Pharmaceutical Microbiology Resources (http://www.pharmamicroresources.com/)


No comments:
Post a Comment
Pharmaceutical Microbiology Resources