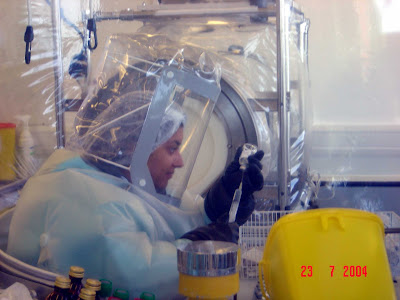
Image: Antibiotic-resistant bacteria, such as Staphylococcus aureus, abound in our wastewater effluents where they could be spreading the resistance gene to other (pathogenic) bacteria. Scientists have now begun to explore ways of preventing this via optimal disinfection processes | Photo courtesy: Prawny on Pixabay
Scientists map the degradation of antibiotic resistance gene mecA by common disinfectants to find ways to minimize the spread of resistance in waterbodies
Antibiotic-resistant bacteria have become a global threat today, owing in part to the efficiency with which resistance spreads among them. Some of this spread happens in waterbodies—and our wastewater systems are no exception. A group of scientists from Korea and the US has now conducted some of the groundwork needed to optimize disinfection processes and minimize the spread of antibiotic resistance through waterbodies.
For nearly a century, improvement in human healthcare has depended heavily on the efficiency with which we can treat bacterial diseases. But today, antibiotic resistance—the ability of certain mutant super-bacteria to block out antibiotics—poses a major threat to healthcare, food security, and overall social development worldwide, threatening to upend much of the progress our civilization has achieved.

Scientists are now urgently attempting to tackle this problem from various angles. Professor Yunho Lee at Gwangju Institute of Science and Technology (GIST), Korea, whose contribution is published in the American Chemical Society’s Environmental Science and Technology, is looking at it from the point of view of his field of research—wastewater treatment. “Bacteria, including antibiotic-resistant bacteria and their resistance genes, abound in various aquatic environments. These are therefore dangerous breeding grounds for antibiotic resistance, where through a process called horizontal gene transfer, resistant bacteria could transfer the resistance gene to other bacteria, which could then increase the antibiotic resistance levels among the members of the bacterial community, including pathogens. We could reduce this occurrence, however, if we determined which disinfectants and how much of them could safely and efficiently kill the resistant bacteria and gene in our drinking water and wastewater effluents.”
As an initial step towards achieving this, Prof. Lee and his team studied the effects of various amounts of chlorine, ozone, and ultraviolet radiation on the degradation of both extracellular and intracellular (contained within bacteria) methicillin (a type of penicillin) resistance gene, mecA, of the bacteria Staphylococcus aureus in water. Based on high resolution observations using scanning electron microscopy and an analysis of the effect of the disinfectants on the reaction dynamics and cell structure, the scientists developed a reaction kinetics model for each disinfectant versus mecA in addition to a method for measuring the degradation rates. Their experiments verified the effectiveness of their models and method.
“Our findings are a key step in determining the optimal conditions for wastewater disinfection process operations for eliminating mecA and mitigating the spread of antibiotic resistance through our municipal wastewater systems,” says Prof. Lee. “In this way, our research significantly contributes to public health protection against infection by antibiotic-resistant bacteria.”
Moreover, Prof. Lee is hopeful that their models can be applied to other segments of double stranded DNA as well, such as those of certain viruses. Thus, newer approaches like these could hopefully lead to sustainable solutions to the looming antibiotic resistance problem and more in the near future.
Posted by Dr. Tim Sandle, Pharmaceutical Microbiology Resources (http://www.pharmamicroresources.com/)