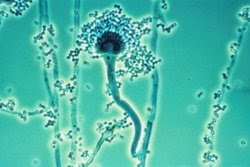
Aspergillus
fumigatus is a common fungus; it grows in many places including soil, plant
matter, and dust around the world. It can also invade the human body. While
most healthy people can eliminate A. fumigatus, the fungus can cause the
disease known as aspergillosis in people with compromised immune systems.
A. fumigatus can bind to a protein in epithelial cells of the lungs, and evade elimination by taking up residence in phagosomes. Scientists from Leibniz Institute for Natural Product Research and Infection Biology have recently investigated how this pathogenic fungus disrupts a natural protective response in the lungs. The findings have been reported in Cell Host & Microbe (see: “Aspergillus fumigatus hijacks human p11 to redirect fungal-containing phagosomes to non-degradative pathway”).

Lung epithelial
cells form a crucial barrier against pathogens in the air, including fungal
spores. While these cells are not specialized pathogen destroyers like some
immune cells, they can still surround foreign material and invaders, and lock
them into compartments called phagosomes. The phagosome undergoes a maturation
process, and the trapped invaders are eliminated.
The study has
shown that fungal spores can alter this defensive response. A fungal protein
made by A. fumigatus called HscA can bind to a human protein called p11,
which triggers a series of events that stops the phagosome from degrading the
fungus.
When the
researchers eliminated the p11 protein, fungal spores in phagosomes are
destroyed. If the fungal protein, HscA is switched off, the fungal spores are
still destroyed. However, if the fungal and human proteins are functioning
normally, the phagosomes never mature and the fungal spores are not destroyed.
The investigators found that the fungi that remained in the immature phagosomes
formed extensions called hyphae, and some spores were also released from the
cell to cause infection in neighboring cells.
The researchers
also found that the same mechanisms were at work in different immune cells.


No comments:
Post a Comment
Pharmaceutical Microbiology Resources